Etiology: Mycoplasma pulmonis is pleomorphic bacterium lacking a cell wall. This organism can induce a chronic pulmonary disease syndrome. Cilia-associated respiratory (CAR) bacillus is a frequent co-pathogen with M. pulmonis.
Incidence: Although the incidence of infection is rare, the significance when present is high, often leading to fulminating respiratory disease.
Transmission: Transmission by direct contact with infected secretions has been reported. M. pulmonis can also be transmitted transplacentally.
Clinical Signs: Disease is often subclinical. Adverse environmental factors such as high cage ammonia levels, and/or the acquisition of primary viral or bacterial respiratory pathogens can activate subclinical infections. Early signs of overt disease may include a red (porphyrin) oculonasal discharge, nasal stridor, sneezing and snorting. Other clinical signs include anorexia with weight loss, rough hair coat and hunched posture.
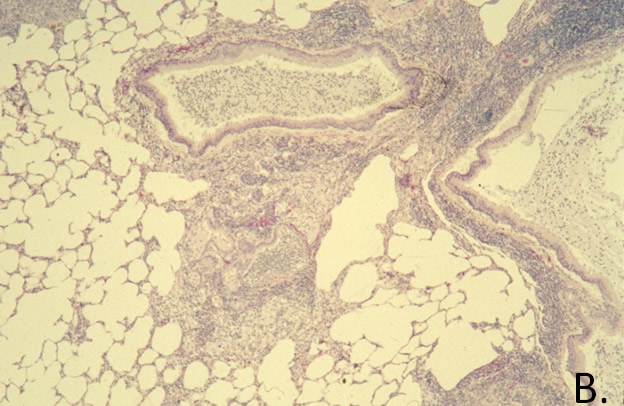
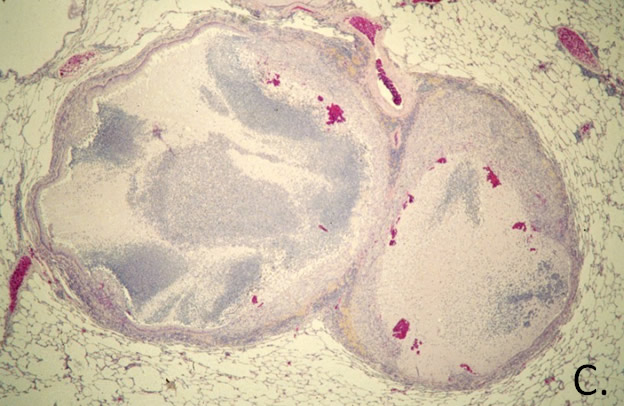
Pathology: A purulent discharge may be found on the nasal mucosa and within the tympanic bullae. Purulent exudate can be found in the trachea and in the bronchi. In some cases, the lungs may be grossly normal. In pneumonic lungs yellow foci of bronchiectasis and red to grey areas of consolidation are found in the lung (A.). Infected uteri may contain fluid in the horns and oviduct (hydrosalpinx). Microscopic examination of the lungs may show peribronchiolar lymphoid hyperplasia (B.). A purulent bronchopneumonia and ectatic bronchioles (C.) may also be present. Care should be taken not to confuse the normal bronchiole-associated lymphoid tissue (BALT) with a lesion of mycoplasmosis.
Diagnosis: MFI or IFA are commercially available for serological screening for Mycoplasma pulmonis infections. PCR assays on nasopharyngeal or tracheal samples are also used for diagnosis.