Etiology: Salmonella are Gram-negative, toxin-producing, invasive, enteric bacteria. The most common serotype of Salmonella enterica to infect mice is serovar Typhimurium.
Incidence: The incidence of salmonellosis is rare in research mice.
Transmission: The disease is spread by fecal-oral transmission.
Clinical Signs: Disease in susceptible colonies may be manifest only as acute death with no clinical signs of infection. Moderate morbidity characterized by hunched posture, anorexia, lethargy, and high to sporadic mortality may be observed in weanlings and in females in late gestation. Diarrhea may or may not be present. The disease will become endemic, with periodic cycling of overt disease symptoms such as acute deaths, chronic low fertility, fetal reabsorption, or abortion.
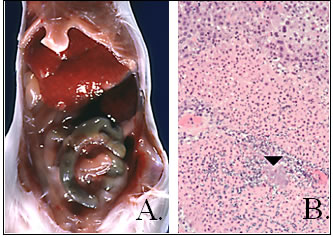
Pathology: In acute infections, the spleen may be enlarged 2 to 3 times normal size. Lesions in the small intestine consist of mucosal congestion and edema with thrombosis of the mesenteric vasculature. In sub-acute infections, multiple white to yellow foci occur in the liver, spleen is enlarged, and mesenteric lymph nodes may be enlarged and edematous (A). Histopathologic examination may reveal multifocal necrotizing splenitis and hepatitis, with necrotic foci often accompanied by colonies of bacteria (arrowhead, B.).
Diagnosis: A history of the disease outbreak, decreased fecundity in breeding colonies, gross lesions, and identification of wild rodent exposure can be suggestive of salmonellosis. A definitive diagnosis is determined by culture of liver and spleen (in acute cases), feces, mesenteric lymph node, and ileal homogenates (in subacute cases) on selective media such as selenite, brilliant green and MacConkey’s agar with serotyping of the isolate using PCR.
Public Health Significance: Humans ingesting Salmonella contaminated food or water may experience a transient diarrhea. Children or immunocompromised adults may experience more severe disease [2]. The disease in humans is reportable.