Etiology: Encephalitozoon cuniculi is an obligate intracellular, Gram-positive, microsporidian parasite. Multiple strains have been identified.
Incidence: Incidence of infection is low.
Transmission: E. cuniculi is shed in the urine and is transmitted through the ingestion of spores. Inhalation of the spores is also thought to occur. Spores are excreted in the urine for up to three months following infection. Vertical transmission has also been reported in rabbits.
Clinical Signs: In acute infections, usually there are no clinical signs. However, in chronic infections there may be neurologic signs including torticollis, depression, tremors, and paresis. Uveitis with cataracts has also been reported.
Diagnosis: Diagnosis may be made by serologic detection of antibody via MFI and indirect fluorescent antibody tests (IFA). PCR of kidney tissue can be used to diagnose E. cuniculi. Diagnosis is also provided by histopathologic demonstration of organisms. Encephalitozoon stains eosinophilic with hematoxylin and eosin stains but is Gram-positive (black arrowhead, A.) and refractile when viewed with polarized light.
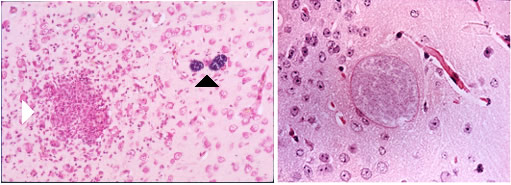
Diagnostic Morphology: Spores measure 2.5 x 1.5 µm (oval) with a thick wall.
Pathology: In acute cases the kidneys are swollen. Chronic lesions are more commonly seen and include multifocal, pinpoint, white, pitted areas on the surface of the kidneys. Histological examination of kidneys reveals granulomatous nephritis with spores in the tubular epithelia, interstitium, or in tubular lumens. Examination of brain tissue reveals granulomatous meningoencephalitis with astrogliosis and perivascular lymphoid infiltrates (A.) Organisms (B.) may be within glial cells or in granulomas. Other tissues affected include the liver, lungs, and heart.
Please see rabbit Parasitic Diseases for more detailed information.
Public Health Significance: Encephalitozoon cuniculi has been identified in immunosuppressed humans [1].
1. Weber, R., et al., Cerebral microsporidiosis due to Encephalitozoon cuniculi in a patient with human immunodeficiency virus infection. N Engl J Med, 1997. 336(7): p. 474-8.